Metabolic Syndrome And Dementia: A Study Reveals A Significant Link
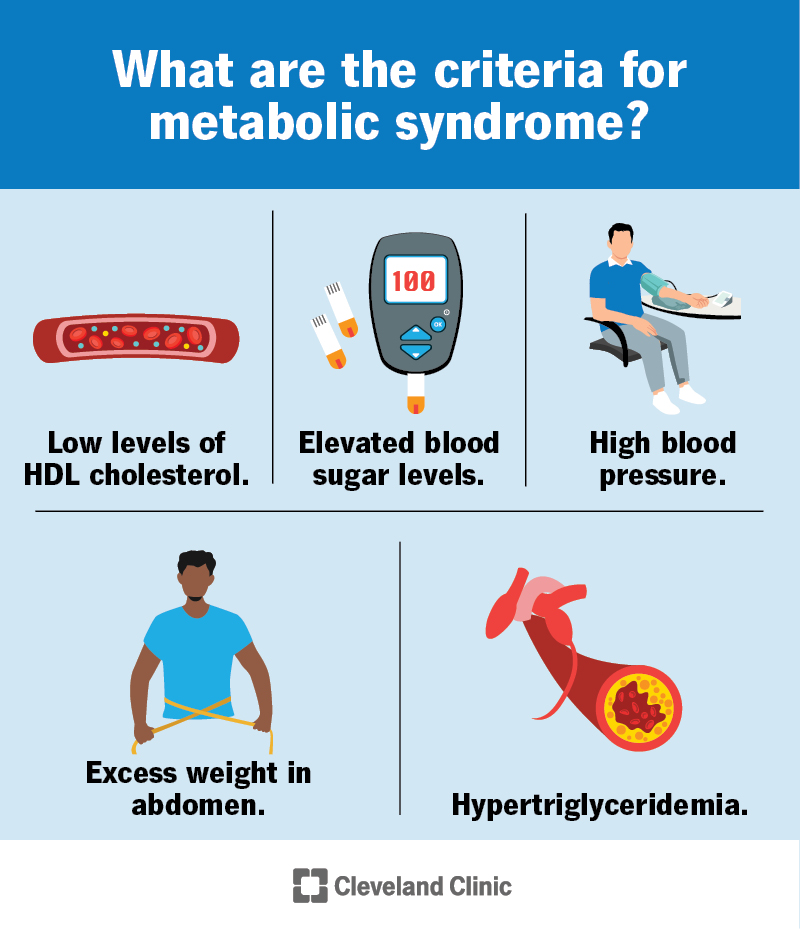
Table of Contents
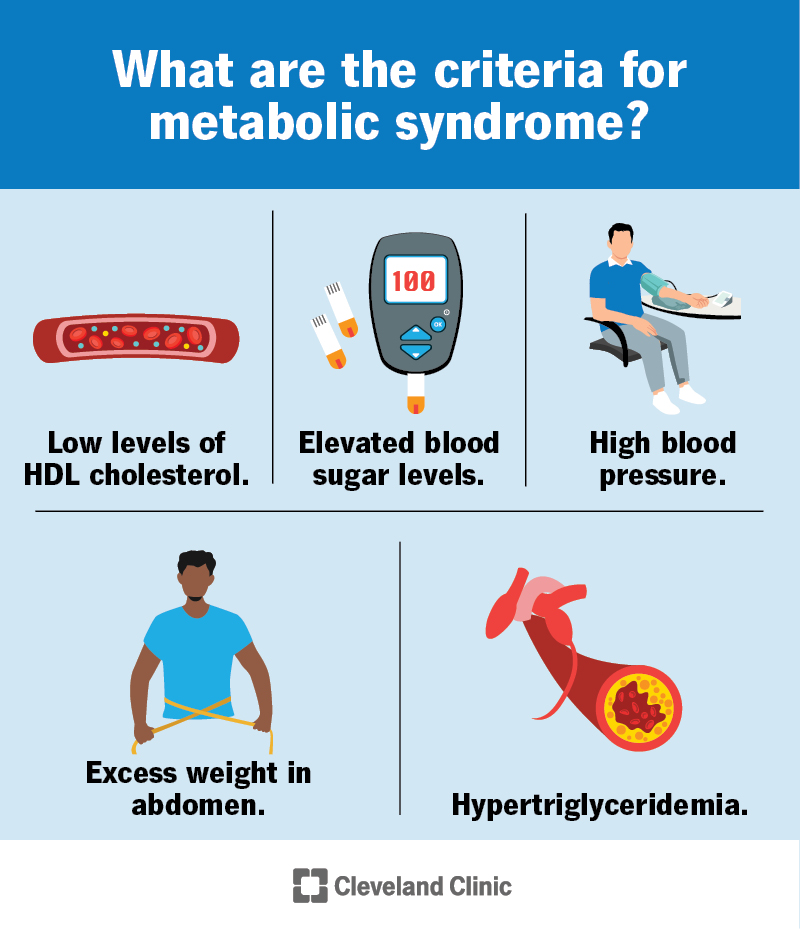
Metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. Key components include:
- High blood pressure (hypertension)
- High blood sugar (hyperglycemia)
- Excess abdominal fat (central obesity)
- High triglycerides
- Low high-density lipoprotein (HDL) cholesterol ("good" cholesterol")
Emerging research strongly suggests a connection between MetS and an increased risk of developing dementia, a debilitating condition characterized by cognitive decline and memory loss. This article aims to delve into this significant link, examining the contributing factors and outlining strategies for mitigation.
Understanding the Components of Metabolic Syndrome and Their Impact on the Brain
Several components of MetS directly contribute to brain health deterioration and increased dementia risk.
Insulin Resistance and its Neurological Consequences
Insulin resistance, a core feature of MetS, impairs the brain's ability to utilize glucose efficiently. This impairment has profound neurological consequences.
- Insulin's role in brain glucose metabolism: Insulin facilitates glucose uptake into brain cells, providing essential energy for neuronal function. Insulin resistance disrupts this process, leading to energy deficits and impaired neuronal activity.
- Impact on amyloid-beta plaques and tau tangles: Hyperinsulinemia (excessively high insulin levels) is linked to increased production and deposition of amyloid-beta plaques and tau tangles, hallmarks of Alzheimer's disease.
- Neuroinflammation: Insulin resistance triggers chronic, low-grade inflammation in the brain, contributing to neuronal damage and cognitive impairment. This neuroinflammation further accelerates cognitive decline.
Hypertension and its Contribution to Cerebral Vascular Disease
High blood pressure damages blood vessels throughout the body, including those in the brain. This damage leads to a range of cerebrovascular diseases.
- Mechanisms of cerebrovascular damage: Hypertension causes structural changes in cerebral blood vessels, reducing cerebral blood flow and increasing the risk of stroke. White matter lesions, often visible on brain scans, are a common consequence of chronic hypertension.
- Increased risk of stroke and vascular dementia: Stroke, caused by interrupted blood supply to the brain, is a major cause of vascular dementia. Hypertension significantly elevates the risk of both.
Dyslipidemia and its Role in Atherosclerosis and Cognitive Decline
Abnormal lipid levels (dyslipidemia) contribute to atherosclerosis, a process of plaque buildup in the arteries. This plaque restricts blood flow, starving the brain of oxygen and nutrients.
- High cholesterol, triglycerides, and low HDL: High levels of LDL cholesterol ("bad" cholesterol) and triglycerides, coupled with low HDL cholesterol, accelerate atherosclerosis.
- Impact on cognitive function: Reduced blood flow to the brain due to atherosclerosis impairs cognitive function, increasing the risk of dementia, including vascular dementia and Alzheimer's disease.
Studies Linking Metabolic Syndrome and Dementia: A Review of the Evidence
Numerous studies have established a strong link between MetS and increased dementia risk.
Epidemiological Studies
Large-scale epidemiological studies consistently demonstrate a correlation between MetS and increased dementia risk.
- Framingham Heart Study: This landmark study showed a significant association between MetS and an increased risk of cognitive decline and dementia.
- Numerous cohort studies: Multiple longitudinal studies have replicated these findings, confirming the robust association between MetS and dementia across diverse populations. These studies typically report increased relative risks and odds ratios for dementia in individuals with MetS.
Mechanisms Linking Metabolic Syndrome and Dementia
The exact mechanisms linking MetS to dementia are complex and multifaceted, but several pathways are implicated.
- Inflammation: Chronic inflammation, a consequence of insulin resistance and other MetS components, damages brain cells and contributes to neurodegeneration.
- Oxidative stress: Metabolic dysfunction leads to increased oxidative stress, further damaging brain cells and accelerating cognitive decline.
- Neurovascular dysfunction: Hypertension and atherosclerosis impair blood flow to the brain, reducing oxygen and nutrient delivery and leading to neuronal damage. This neurovascular dysfunction is a key mechanism underlying vascular dementia.
- Amyloidogenesis and tau hyperphosphorylation: Insulin resistance and inflammation contribute to the accelerated formation of amyloid plaques and the hyperphosphorylation of tau proteins which are hallmarks of Alzheimer's disease pathology.
Lifestyle Modifications and Preventative Strategies
Adopting a healthy lifestyle is crucial for mitigating the risk of both MetS and dementia.
Dietary Changes
A balanced diet plays a vital role in preventing and managing MetS and reducing dementia risk.
- Mediterranean diet: This diet, rich in fruits, vegetables, whole grains, and healthy fats, has been shown to improve metabolic health and protect against cognitive decline.
- Weight management: Maintaining a healthy weight reduces the burden on the body's metabolic systems.
Exercise and Physical Activity
Regular physical activity significantly improves metabolic health and reduces dementia risk.
- Types of exercise: Aerobic exercise, such as brisk walking, swimming, or cycling, is particularly beneficial. Strength training is also crucial for maintaining muscle mass and overall health.
- Frequency: Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week.
Other Lifestyle Factors
Other lifestyle factors influence both MetS and dementia risk.
- Sleep quality: Prioritize adequate and restful sleep.
- Stress management: Implement effective stress reduction techniques, such as meditation or yoga.
- Smoking cessation: Quit smoking to significantly improve cardiovascular and cognitive health.
Conclusion: Taking Action Against Metabolic Syndrome and Dementia
The strong evidence linking metabolic syndrome and dementia underscores the importance of early detection and intervention. Managing metabolic syndrome effectively reduces the risk of developing dementia. By adopting a healthy lifestyle that includes a balanced diet, regular exercise, stress management, and smoking cessation, individuals can significantly reduce their risk of both MetS and dementia, protecting their brain health and preventing cognitive decline. Consult your healthcare provider for screening and personalized strategies for managing metabolic syndrome and reducing your risk of dementia. Taking proactive steps towards a healthier lifestyle is crucial for preventing cognitive decline and preserving your brain health for years to come.
Featured Posts
-
 Weeks Away Eurovision 2025s Potential Winners
Apr 25, 2025
Weeks Away Eurovision 2025s Potential Winners
Apr 25, 2025 -
 Rws Ka Ywkryn Pr Hmlh Dwnld Trmp Ky Raye Awr Ealmy Rdeml
Apr 25, 2025
Rws Ka Ywkryn Pr Hmlh Dwnld Trmp Ky Raye Awr Ealmy Rdeml
Apr 25, 2025 -
 Examining The Difficulties In Elon Musks Robotaxi Development
Apr 25, 2025
Examining The Difficulties In Elon Musks Robotaxi Development
Apr 25, 2025 -
 Ashton Jeanty To The Bears A Realistic Possibility
Apr 25, 2025
Ashton Jeanty To The Bears A Realistic Possibility
Apr 25, 2025 -
 Ukrayina Ta Tramp Klyuchovi Zmini V Yogo Vislovlyuvannyakh Pro Viynu
Apr 25, 2025
Ukrayina Ta Tramp Klyuchovi Zmini V Yogo Vislovlyuvannyakh Pro Viynu
Apr 25, 2025
