The Rise Of Deadly Fungi: A Looming Public Health Crisis

Table of Contents
The Growing Threat of Drug-Resistant Fungi
The increasing prevalence of drug-resistant fungi represents a major challenge in combating these deadly infections. The rise of resistant strains is directly linked to several key factors, creating a perfect storm for more severe and difficult-to-treat fungal diseases.
Increased Antibiotic Use and Resistance
The overuse and misuse of antibiotics have inadvertently created a breeding ground for drug-resistant fungi. Antibiotics disrupt the delicate balance of the human microbiome, allowing opportunistic fungi to thrive and develop resistance mechanisms. This contributes to the rise of deadly fungi infections that are harder to treat and more likely to result in severe outcomes.
- Increased hospital stays: Patients with drug-resistant fungal infections require prolonged hospitalizations, increasing healthcare costs and placing strain on healthcare systems.
- Higher mortality rates: Drug resistance significantly increases the risk of death from fungal infections.
- Prolonged recovery times: Treatment of resistant fungi is often complex and lengthy, leading to extended recovery periods and diminished quality of life.
- Increased healthcare costs: The expense of treating drug-resistant fungal infections is substantially higher due to longer hospital stays, specialized medications, and intensive care requirements.
Specific examples of drug-resistant fungi causing significant concern include Candida auris, known for its multi-drug resistance and rapid spread in healthcare settings, and Aspergillus fumigatus, a common environmental fungus that can cause life-threatening infections in immunocompromised individuals.
Failure of Existing Antifungal Drugs
The arsenal of effective antifungal drugs is limited, and the development of new antifungals has lagged behind the development of antibacterial agents. This shortage, coupled with increasing resistance, makes treating deadly fungal infections increasingly challenging.
- Need for research and development of new antifungals: Urgent investment in research is needed to discover and develop new antifungal agents with novel mechanisms of action.
- Limitations of current treatment options: Existing antifungal medications often have limited efficacy against resistant strains, leading to treatment failure and worse outcomes.
- Challenges in drug delivery: Delivering antifungal drugs effectively to the site of infection can be difficult, especially in deep-seated infections.
The mechanisms of antifungal resistance are complex and involve various adaptations within the fungus, including changes in drug targets, increased drug efflux, and enzymatic inactivation of the drug. Developing new drugs that overcome these resistance mechanisms is a significant hurdle in the fight against deadly fungi.
Environmental Factors Contributing to Fungal Growth
Changes in the environment are significantly contributing to the expansion of fungal habitats and increased exposure to potentially deadly fungi.
Climate Change and Fungal Proliferation
Rising global temperatures and increased humidity create ideal conditions for the growth and spread of many fungal species. Climate change is extending the growing seasons for fungi and facilitating the spread of previously geographically restricted species.
- Expansion of fungal habitats: Warmer temperatures and altered precipitation patterns are expanding the geographical range of many fungal species, increasing human exposure.
- Increased incidence of fungal spores in the air: Higher temperatures and humidity can lead to a higher concentration of fungal spores in the air, increasing the risk of inhalation and infection.
- Longer fungal growing seasons: Longer periods of favorable weather conditions allow fungi to proliferate more extensively, increasing the overall fungal biomass and spore production.
Certain fungal species, such as those causing histoplasmosis and coccidioidomycosis, are known to thrive in warmer, drier climates, and their prevalence is expected to increase with ongoing climate change.
Deforestation and Habitat Loss
Deforestation and habitat disruption alter ecosystems, potentially increasing human exposure to previously isolated fungal species and disrupting natural checks and balances on fungal populations.
- Increased human-animal interactions: Habitat encroachment brings humans into closer contact with animals that may harbor potentially pathogenic fungi.
- Exposure to novel fungal species: The destruction of natural habitats can expose humans to new fungal species, some of which may be highly pathogenic.
- Disruption of ecological balance: Changes in biodiversity can disrupt the complex interactions within ecosystems, potentially leading to an increase in the abundance of certain fungal species.
Deforestation not only alters fungal biodiversity but can also increase the risk of human exposure to deadly fungi through various pathways.
Vulnerable Populations and Increased Risk
Certain populations are disproportionately vulnerable to severe fungal infections due to compromised immune systems or other underlying health conditions.
Immunocompromised Individuals
Individuals with weakened immune systems are at significantly higher risk of developing severe and life-threatening fungal infections. These opportunistic infections can be devastating and difficult to treat.
- Higher mortality rates: Immunocompromised individuals have a much higher mortality rate from fungal infections.
- Increased risk of opportunistic infections: A weakened immune system allows fungi, normally harmless, to cause serious disease.
- Challenges in diagnosis and treatment: Diagnosing fungal infections in immunocompromised individuals can be challenging, and treatment may be more complex and less effective.
Conditions such as HIV/AIDS, organ transplantation, cancer, and autoimmune diseases significantly increase susceptibility to deadly fungi.
Elderly Population
The globally aging population represents a growing segment of the population at increased risk of severe fungal infections.
- Weakened immune systems: Immune function naturally declines with age, increasing vulnerability to opportunistic infections.
- Increased co-morbidities: Older adults often have multiple underlying health conditions that further compromise their immune systems.
- Challenges in treatment: Older individuals may be less tolerant of antifungal medications and more prone to adverse effects.
Age-related changes in the immune system, coupled with increased prevalence of chronic diseases, make the elderly particularly susceptible to the serious consequences of deadly fungi.
Improving Diagnosis and Treatment of Deadly Fungi
Improving diagnostic capabilities and developing novel antifungal agents are crucial for effectively addressing the threat of deadly fungi.
Rapid Diagnostic Techniques
Rapid and accurate diagnosis is crucial for timely intervention and improved patient outcomes. Current diagnostic methods often lack speed and sensitivity, hindering effective treatment.
- Molecular diagnostics: Techniques such as PCR offer rapid and sensitive detection of fungal pathogens.
- Advanced imaging techniques: Imaging modalities can aid in identifying the location and extent of fungal infections.
- Improved laboratory tests: Developing more accurate and rapid laboratory tests is essential for improving diagnosis.
Faster and more reliable diagnostic methods are critical for improving patient care and reducing mortality rates associated with deadly fungi.
Development of Novel Antifungal Agents
The development of new antifungal drugs with novel mechanisms of action is essential to combat the growing problem of drug resistance.
- Targeting fungal-specific pathways: Identifying and targeting unique fungal pathways can lead to the development of drugs with improved efficacy and reduced toxicity.
- Combinatorial therapies: Combining different antifungal drugs can enhance efficacy and reduce the development of resistance.
- Drug repurposing: Investigating existing drugs for their potential antifungal activity can accelerate the development of new treatments.
Ongoing research efforts focused on antifungal drug discovery are crucial for staying ahead of the evolving threat of drug-resistant deadly fungi.
Conclusion
The rise of deadly fungi presents a formidable challenge to global public health. The convergence of factors like antibiotic resistance, climate change, and an aging population is creating a perfect storm for increased fungal infections. Addressing this crisis requires a multi-pronged approach, including improved diagnostics, development of novel antifungal agents, and public health initiatives aimed at reducing risk factors. We must prioritize research into deadly fungi and invest in preventive measures to mitigate the looming threat of this emerging health crisis. Increased awareness and proactive strategies are crucial to protect vulnerable populations and safeguard public health from the ever-increasing menace of deadly fungi.

Featured Posts
-
 Qwmy Hyrw Aym Aym Ealm Ky 12 Wyn Brsy Pakstan Bhr Myn Tqrybat
May 08, 2025
Qwmy Hyrw Aym Aym Ealm Ky 12 Wyn Brsy Pakstan Bhr Myn Tqrybat
May 08, 2025 -
 Gjranwalh Wlyme Ky Tqryb Myn Dl Ka Dwrh Dlha Jan Bhq
May 08, 2025
Gjranwalh Wlyme Ky Tqryb Myn Dl Ka Dwrh Dlha Jan Bhq
May 08, 2025 -
 Anons Pivfinaliv Ligi Chempioniv Arsenal Proti Ps Zh Barselona Proti Intera 2024 2025
May 08, 2025
Anons Pivfinaliv Ligi Chempioniv Arsenal Proti Ps Zh Barselona Proti Intera 2024 2025
May 08, 2025 -
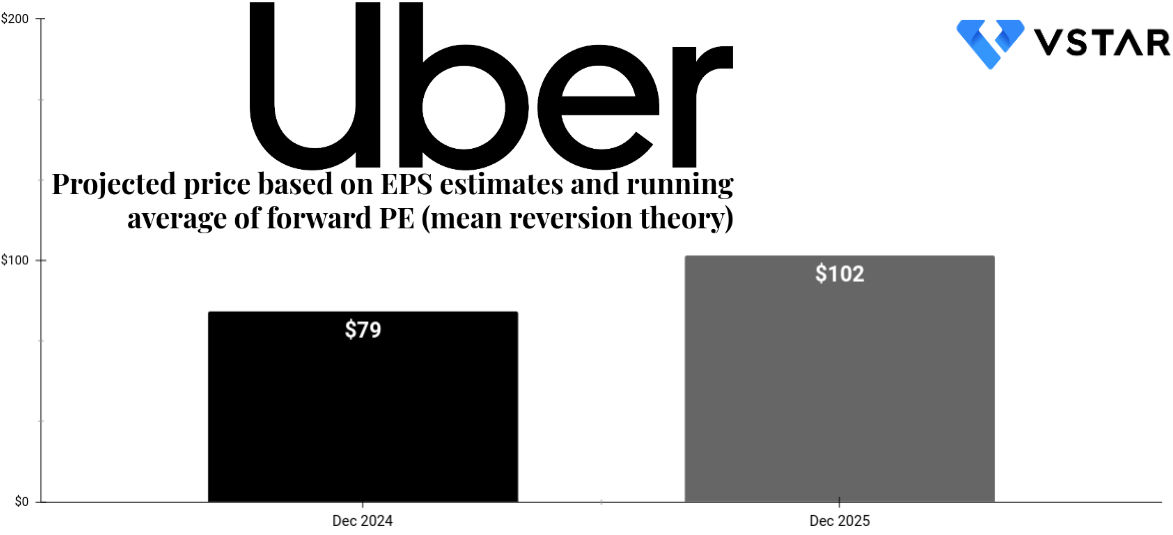 Uber Stock Forecast Will Autonomous Vehicles Drive Growth
May 08, 2025
Uber Stock Forecast Will Autonomous Vehicles Drive Growth
May 08, 2025 -
 First Look At The Stephen Kings The Long Walk Film Adaptation
May 08, 2025
First Look At The Stephen Kings The Long Walk Film Adaptation
May 08, 2025
